In partnership with the
Persistent pain lasts beyond usual healing times. It used to be thought that this is due to ongoing damage, but scientific research has shown that this is unlikely. The pain is more likely to be related to the nervous system (brain and nerves) becoming sensitised, a bit like the volume on your radio being stuck on loud. When this happens, it can be difficult to do your normal activities. It is possible to turn the volume down, but it takes time and effort. This means that quick fixes, such as medications, injections and operations are often unhelpful.
The reason these interventions can be less helpful is that the nervous system takes short cuts to improve efficiency. This is affected by past experiences, thoughts, expectations and emotions, not only tissue damage/injury. A good example of this is someone with low back pain, where bending the back causes pain. To improve efficiency, your nervous system predicts that bending your back will hurt, even if you are not receiving pain messages from the structures in the back. This is not a conscious decision and is completely normal, although it may be unhelpful in many circumstances.

The pain symptoms often lead to people becoming less active, but this means that the muscles get weaker and sleep quality gets worse. The symptoms and reducing activity is often referred to as a vicious cycle. Pain can also impact on your relationships, as you may feel less patient, experience negative thoughts, feel your mood is affected or less able to do the things you used to do. It can be difficult to adapt, but there are positive steps you can take to improve your situation, including being referred to the Circle MSK service.
It can be difficult to achieve a diagnosis of persistent pain. People often tell us that they meet a number of clinicians in search of a medical test, to find out why they are experiencing their symptoms. Unfortunately there are no tests that are able to diagnose persistent pain, although sometimes scans, blood tests or x-rays can be used to exclude other causes. This is because the symptoms often relate to a nerve sensitivity, rather than an injury. However, in many cases these tests are not useful and do not add any extra information. The diagnosis is most effectively made by meeting with a clinician, this could be a pain physiotherapist, nurse or Doctor, who can do a thorough assessment, by listening to your story (how your symptoms developed, how you manage day to day, how work is affected) and looking at how you move.
The videos below explain how persistent pain can develop:
Many people with persistent pain tell us they feel like they are caught in a ‘pain trap’. Pain traps are a term used to describe factors that can contribute towards your pain symptoms. Examples of these include factors that you may be able to influence, such as pushing yourself through pain excessively. External factors, such as stress may also contribute to symptoms. Some examples of how your thoughts, feelings and emotions relate to your symptoms are shown in the sections below.
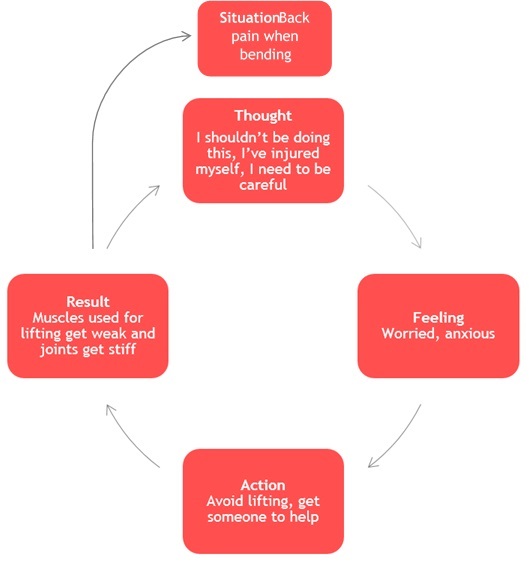
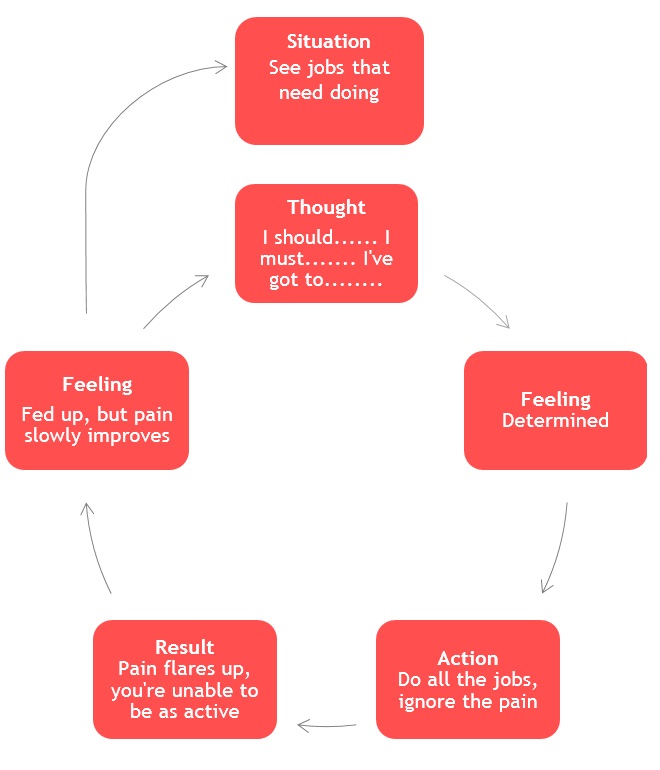
Healthcare professionals may have used the term vicious cycle to describe your symptoms and activity, but what does this mean? Below are two types of vicious cycle and most people tend to fit into one of these activity types. It is important to realise that both are completely normal and natural responses to ongoing pain problems, and although they may feel helpful, this benefit is only short term and may contribute to making things worse in the long run.
You may recognise your own thought processes in one or both of the above vicious cycles. There are specific strategies you can put in place to counter balance these natural cycles, but the exact approaches can vary from person to person.
Negative automatic thoughts are something that we can all relate to! These are the automatic thoughts that automatically pop into our heads, quite uninvited and some people may notice these more often.
Examples of negative automatic thoughts are:
‘Why does this always happen to me?’
‘I know exactly what he/she is thinking……’
‘I will never get out of this mess’
These thoughts are a constant stream in everyone, however, some people may pay more attention to them than others. Taking time to notice that these automatic thoughts can impact on how you feel can be important, as these thoughts are rarely helpful. If you find yourself dwelling on these thoughts, it would be sensible to speak with your GP or health professional. If you have an ongoing pain problem, our pain team may be able to help, there are specific strategies you can put in place to manage the impact they are having on your daily life.
Our team of specialist physiotherapists or osteopaths can support you via a range of services designed to meet your needs, such as our multi-disciplinary pain team, pain management programme, Clinical Psychology, Back Skills Training or Physiotherapy/Osteopathy. Any improvement requires commitment, both in terms of being open new ideas and the time investment in attending sessions

Self-Help, or Self-Management is essential in the management of persistent pain, as it helps people reduce their reliance on healthcare professionals and take control of the management of your symptoms.
We aim to work with you to reduce your pain and improve quality of life. This is involves supporting you to take an active role in your own well-being. Research has shown that self-management of persistent pain is beneficial in the long term.
Self-Management however, is an important step and offers a positive way to improve quality of life. This explores how you may be able to live a normal life, despite a change in health. This usually includes pacing activities, exercise, sleep management, positive thinking, goal setting and relaxation techniques.
Benefits vary for each person and can also vary according to how well you engage and are willing to try each technique, sometimes people can become over-reliant on healthcare professionals to manage their symptoms. This helps develop a strategy that works for specifically for you.
Specialist physiotherapists identify reasons for lack of progress in rehabilitation, such as fear avoidance of movement or unhelpful patterns of over- and under-activity.
Treatment can involve gradual exercise, building up overall activity and relaxation techniques, to manage you pain and improve function.
Back skills training is an evidence based approach to the management of low back pain, to find out more about this, please click here
The Circle Integrated Care pain management programme is a multi-disciplinary team approach including pain education, psychology, and physical strategies for managing pain.
The group runs for 2 hours once per week for 6 consecutive weeks. These sessions provide you with the tools to manage your symptoms – it’s important to remember that you have to do the work!
There are free online resources, which offer a taster of what these sessions include, and can be found on the retrainpain.org website
The pain nurse team can offer medication review to optimise your pain medications. This in some cases can often mean reducing the number of medications you are taking which are not reducing your pain symptoms, but may have unwanted side-effects.
Psychologists are experts in helping people cope with the thoughts, feelings and behaviours that accompany chronic pain. You may discuss your physical and emotional health. The psychologist may ask about the pain you experience, where and when it occur and factors that affect it. They may also discuss any worries or stresses, including those related to your pain and help you to develop alternative coping strategies to improve your quality of life.
You also may be asked to complete a questionnaire that allows you to record your own thoughts and feelings about your pain.
Pathway through Pain is an online Pain Management Programme (PMP). This digital PMP allows patients the flexibility to follow the course at convenient times and at a pace that suits them. This course has empowered people to do more, feel better and reduce the intensity of their pain.
The programme supports patients through the challenges of everyday pain management via instructional videos, as well as providing advice to keep you feeling supported and motivated.
To find out more please click here.
Consultants in pain are consultant anaesthetists, who have taken additional training in pain interventions. The use of interventions can be useful when there is a potential root cause for the symptoms. This could be reduced space around a specific nerve, which matches with the area you experience symptoms. The interventions most often relate to an injection and in many cases may provide temporary relief and are therefore not seen as a long term treatment approach.
Pain interventions rarely have a role to play if you are experiencing widespread pain symptoms and are usually offered following the trial of other active treatment approaches, such as physiotherapy, pain management programmes and trials of appropriate medications.
There are a range of websites where further information can be sought, see below
Action on Pain Helpline: 0845 603 1593 | www.action-on-pain.co.uk
Away with Pain: www.awaywithpain.co.uk
The British Pain Society: 020 7269 7840 | www.britishpainsociety.org
Fibromyalgia Association UK Helpline: 0844 887 2444 | www.fmauk.org
FibroAction: 0844 443 5422 | www.fibroaction.org
International Association for the Study of Pain (IASP): www.iasp-pain.org
Pain toolkit: www.paintoolkit.org
Pain Concern Helpline: 0300 123 0789 | www.painconcern.org.uk
Pain UK: www.painuk.org | Twitter @pain_uk
Versus Arthritis: www.versusarthritis.org