GTPS describes pain in the outer aspect (lateral) of the hip.
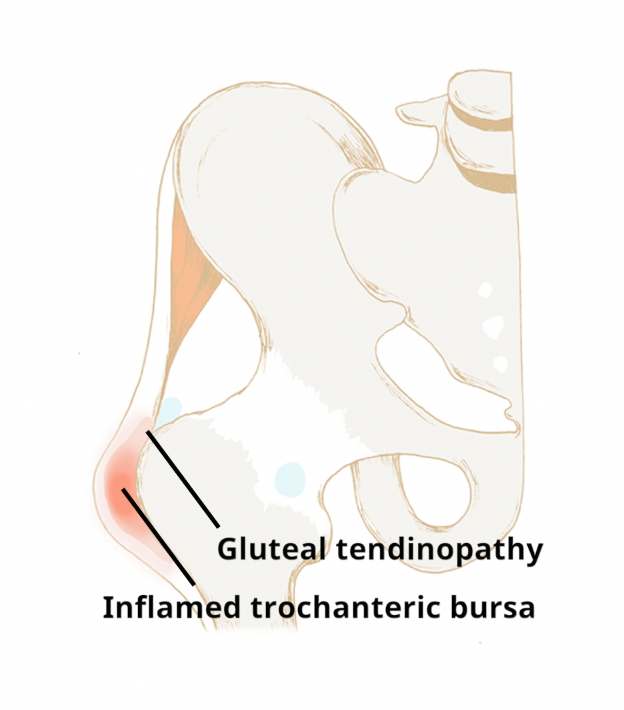
It is usually caused by damage to the gluteal (buttock muscle) tendons. This gluteal tendon damage (tendinopathy) causes pain and weakening of the fibres of the strong band of tissue which attaches the gluteal muscles to bone of the outer hip. It is sometimes associated with inflammation in the fluid filled sac which lies on the outside of the hip, known as the trochanteric bursa. These conditions often co-exist and are termed greater trochanteric pain syndrome (GTPS).
Normally there is a gradual onset, thought to result from excessive friction between the greater trochanter (bony prominence on the outside of the hip) and the gluteal tendons or iliotibial band.
The following factors may predispose to developing excessive friction:
- Direct trauma to the side of the pelvis
- Weak hip abductor muscles
- Sudden increase in activity levels such as cycling or running
- Prolonged standing
- High body mass index (BMI)
- Associated low back pain or arthritis of the lower limb resulting in weakness and fatigue to the hip muscles
How is greater trochanteric pain syndrome treated?
In the majority of cases, GTPS can be managed very effectively by following a regular exercise routine:
Modifying aggravating activities
This does not mean that you will have to stop cycling, running etc. However, the trochanteric bursa and gluteal tendon may need 4-6 weeks of relative rest initially to settle symptoms while you work on strengthening the hip abductor muscles (see below).
Activity modification is the key to relief of symptoms. It is essential to remove causative factors for the tendon to heal. This may take several weeks. Examples are reducing time walking or standing, appropriate footwear and weight reduction.
Exercises
Regular exercises to strengthen the hip abductor muscles and tendon.
These are suggested exercises only. If you are at all concerned about whether these exercises are suitable for you or if you experience any pain while doing them, please seek appropriate clinical advice from your GP or Physiotherapist.
Physiotherapy
Symptoms will normally settle following a period of activity modification and home exercises. However, in persistent cases your clinician may consider a referral for physiotherapy.