In partnership with the
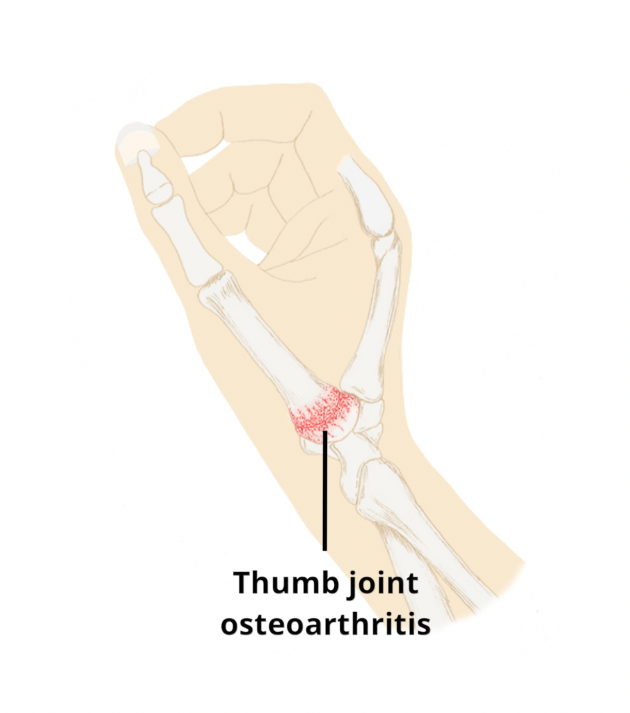
This is the name given to the joint changes, related to age, which cause pain and stiffness at the base of the thumb (next to the wrist). The age-related changes cause stiffness of this joint as well as the soft tissues around the joint. This can cause swelling, and pain. There is increased chance of this happening if you have the following:
- Previous joint damage (from trauma or other conditions such as such as gout and rheumatoid arthritis)
- Age (risk increases with age)
Family history of thumb arthritis (genetics)
Most commonly a deep pain is felt on the thumb side of the wrist, at the base of the thumb, on movement of the joint.
Fortunately, the presence of thumb CMCJOA does not always cause pain so it is quite possible to be pain free despite reasonably advanced arthritis. In addition, the joint undergoes a ‘’wear and repair’’ cycle so pain can improve spontaneously or with appropriate treatment.
Pain with forcible activity involving the thumb is the most common symptom. Movements involving opposition/ gripping, especially if this involves rotation, such as turning a key in a lock are often aggravating activities. If CMCJ OA becomes more severe the movements of the thumb may become increasingly stiff.
Thumb CMCJ OA can be reliably diagnosed by your doctor or physiotherapist by taking a history of your condition and by conducting a physical examination. The main feature on examination is often a reduced range of movement with associated crepitus ( a crunching noise). Therefore, X-rays and scans are NOT routinely required but may be requested if there is diagnostic doubt or symptoms are severe enough that surgery is being considered.
Non-surgical management
In most cases, the symptoms of thumb CMCJ OA can be managed effectively for a long time by the measures described below.
Avoidance of aggravating activities
If pain has been triggered by an increase in activity, for example gripping a hammer doing DIY , then a period of relative rest will often improve the symptoms.
Ice/heat
If pain is troublesome, using ice or heat may help with pain relief. Please take care not to put ice directly on the skin – use a cloth. Please take care not to burn the skin with temperatures that are too hot, or by leaving the ice or heat for too long on the skin.
Wrist/ thumb splint:
Wearing a thumb spica splint every now and then when performing certain tasks may reduce stresses on the wrist & thumb joint. It is best to wear this at intervals (not all the time) and during painful activities. If worn for too long you can risk increasing joint stiffness or muscle weakness of the CMC joint.
Exercises
Isometric contractions of the muscles such as gripping a tennis ball and holding this grip for 10 seconds at a time, or similar, may help symptoms and to maintain muscle strength.
5Using painkillers when needed:
Anti-inflammatory gels may help ease symptoms and are safer than tablets. As long as you have no medical reason not to use them such as an allergy or asthma, they may help ease the pain. Please consult your pharmacist if doubt.
Over the counter painkillers available from pharmacies may help pain when needed. Paracetamol is the most commonly used painkiller. Anti-inflammatory tablets, such as ibuprofren, can be used but only if there is some swelling in the joint. The following link gives you more information about this treatment option:
Painkillers and NSAIDs | Side-effects, uses, time to work (versusarthritis.org)
Corticosteroid injection therapy
For individuals with thumb CMCJ OA who continue to suffer significant symptoms even though they have tried the treatments described above, a corticosteroid injection can be considered as an option for management. You can read more about local corticosteroid injections here – Steroid Injections | Side-effects, uses, time to work (versusarthritis.org)
Injections are more effective in mild to moderate joint osteoarthritis, than in joints with more severe changes when joint movement is very reduced. Not everyone will be able to have a corticosteroid injection, but you will be assessed in one of our MSK clinics by someone who injects to check if this is an option that will be appropriate for you.
Surgical management
If you have pain that is there all the time that is significantly affecting your hand function and your quality of life – even after trying the treatment options described above – you may be considered for surgery. You would need to have an X-Ray that confirmed having severe osteoarthritis changes in the joint at the base of the thumb. (CMCJ).
There are different options for surgery. One is called a trapeziectomy – where the joint at the base of the thumb is removed. The ligaments in this area are reconstructed. This usually has excellent outcomes. There is also the option of a thumb joint replacement – similar to the concept of a hip or knee replacement surgery (but in the thumb). There is another surgery where they try to fuse the joint (this means that they try to make the joint stiff so that there isn’t much movement in the joint. It is thought that the lack of movement causes the joint to be less painful).