In partnership with the
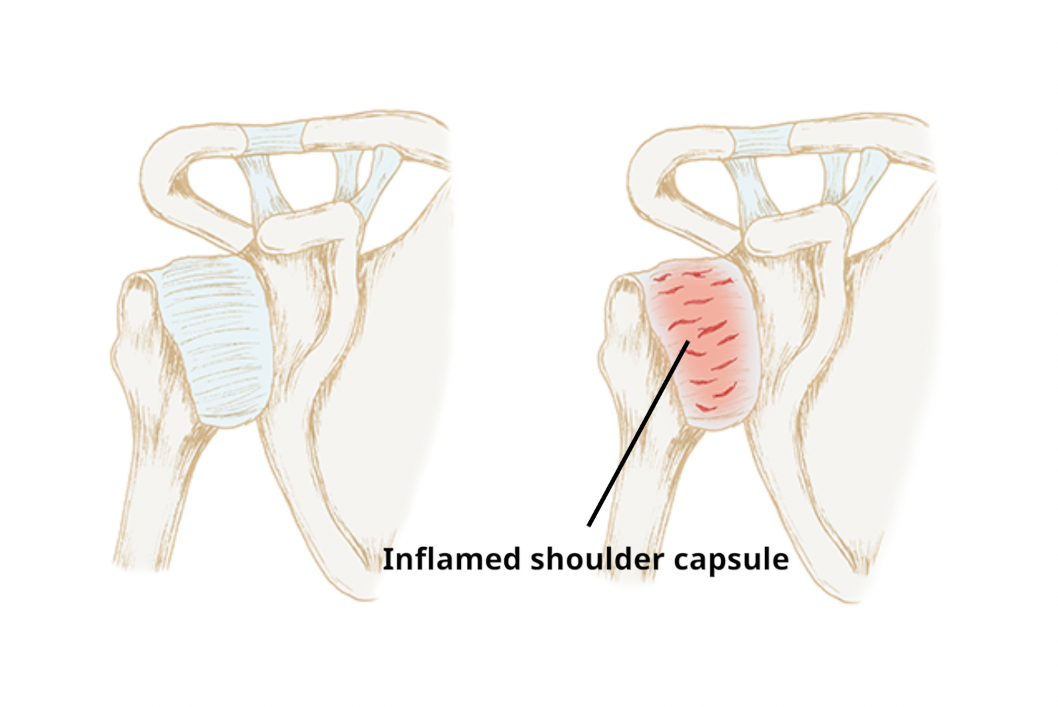
A frozen shoulder (sometimes referred to as shoulder capsulitis) describes a condition in which the soft tissue which encapsulates the joint (joint capsule) becomes painful and inflamed. The process leads to a thickening of the local tissue, which causes the movements of the shoulder to become increasingly stiff (frozen). Fortunately, in most cases, frozen shoulder resolves over 2-3 years.
Frozen shoulder can occur after trauma to the shoulder, but more commonly occurs gradually with no injury or reason. Some people are at greater risk of developing a frozen shoulder:
- Female gender
- Age range 40-60
- Diabetic individuals
Typically, a frozen shoulder has 3 phases:
Stage 1 ('Freezing' phase) - Typically 6-9 months
Inflammation to the joint capsule develops and progresses. The active inflammation often means that the pain is constant rather than movement related and pain levels can be severe and worse through the night. Stiffness to the shoulder movements gradually increases throughout this phase.
Stage 2 ('Frozen' phase) - Typically 4-12 months
Inflammation levels reduce and as such, pain levels become less severe, less constant, and more related to movement. Stiffness to the shoulder movement remains.
Stage 3 ('Thawing' phase) - Typically 12-24
As the tissue within the joint capsule gradually normalises, shoulder flexibility gradually improves as does the pain on shoulder movements. To maximise improvement, it is important to work on exercising the shoulder to regain range of movement and strength during this phase.
A frozen shoulder can be reliably diagnosed by your clinician discussing your symptoms and by conducting a physical examination.
The main feature on examination is increasing restriction of movement at the shoulder. This gradually progresses to involve all movements over a few months (The freezing phase)
X-rays and scans are not routinely required, unless you are considering a form of intervention.
How is a frozen shoulder treated?
A frozen shoulder will improve over time in most cases. Treatment will depend on the stage of the condition and the levels of pain experienced. Initial management will focus on maintaining range of movement and strength.
Exercises. Exercises to help regain flexibility to the affected shoulder joint:
These are suggested exercises only. If you are at all concerned about whether these exercises are suitable for you or if you experience any pain while doing them, please seek appropriate clinical advice from your GP or Physiotherapist.
Using painkillers when needed. Over-the-counter analgesia is available through pharmacies when needed. Paracetamol is most commonly prescribed. Anti-inflammatories, such as Ibuprofen, are also used, but as there is little or no inflammation involved in osteoarthritis these are best avoided without discussing with your GP. Side effects are even more common than with paracetamol so please ensure to take appropriate medical advice. There is a good booklet on the Arthritis Research UK website with information about the various drug options.
Physiotherapy
Physiotherapy can be offered as a treatment option for shoulder pain. This involves a physical assessment and discussion about how your symptoms are impacting your life, followed by developing a treatment plan together. Treatment can include:
-
- Exercises form the mainstay of treatment, with advice regarding exercises to improve flexibility and reduce the sensitivity of the muscles, joints and nerves. Some strength exercises can also be recommended to help improve the strength and function of the tendons and shoulder joint.
-
- Manual Therapy, such as manipulation, mobilisations and soft tissue massage. This usually forms a small portion of your treatment.
Advice to help you speed your recovery and avoid aggravating symptoms.
Corticosteroid injection therapy.
The severe pain which can be a feature of frozen shoulder in stage 1 will often settle with no treatment. However, some individuals experience significant sleep disturbance and limited function. In these circumstances, a corticosteroid injection into the shoulder joint is an effective option to settle pain and expedite recovery. You can read more about local corticosteroid injections here:
Steroid Injections | Side-effects, uses, time to work (versusarthritis.org)
Further treatment options
If the above treatments are not successful in improving your pain and flexibility, other treatments listed below can be considered:
-
- Hydrodilatation Procedure - Involves injecting the shoulder joint with a large volume of fluid (containing saline, steroid and local anaesthetic) to "stretch" the shoulder capsule.
-
- Capsular Release Surgery (keyhole surgery which releases the stiff areas of the shoulder joint capsule)
-
- Manipulation Under Anaesthetic (MUA) Surgery (Manual manipulation of the shoulder joint with the patient asleep)
The two surgical procedures above carry small risks and would be considered only when other treatment options have been exhausted.